Amniotic Fluid Embolism
What is an Amniotic Fluid Embolism?

A Century of Loss
Amniotic fluid embolism was first identified in 1926 through autopsy findings, yet nearly a century later, our understanding of the condition remains limited.
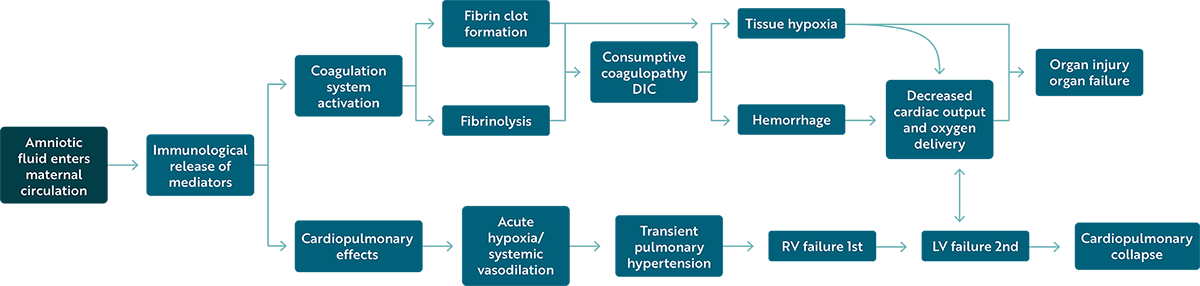
Pathophysiology
Clinical Presentation
Diagnosis
Why Autopsies Are Essential in AFE Diagnosis
A high degree of suspicion is warranted when presumed cases of AFE are reported. The rarity and complexity of AFE can lead to an over-reliance on clinical intuition. Studies suggest that autopsies frequently uncover previously undiagnosed conditions or complications that can lead to alternative diagnoses.
Autopsies allow for:
- Exclusion of other causes
- Identification of histologic findings
- Any concomitant factors
- Evaluation of treatment
- Contribution to medical knowledge
- Closure for loved ones
Why Autopsies Aren’t Always Performed
Cases of maternal death appear to cause a great deal of jurisdictional confusion. Providers often assume a witnessed, natural death in a hospital is ineligible for an autopsy and do not notify the appropriate authorities. Additionally, when cases have been reported, the coroner/ ME has declined the case.
Deaths due to a probable or presumed AFE should be brought in for autopsy as it is a diagnosis of exclusion. It is also the unexpected death of an otherwise healthy individual and is often associated with surgical treatment such as cesarean section or hysterotomy.
Current Funding Opportunities for Maternal Autopsies
The AFE Foundation provides funding for private autopsies in presumed cases of AFE that meet specific qualifications. Hospitals and medical examiners are encouraged to contact the AFE Hotline 1-307-363-2337 to request approval.
The following states have established maternal autopsy programs:
AFE Registry and Biorepository
One of the primary objectives of the AFE Foundation is to advance research to elucidate the etiology and pathophysiology of AFE. Through this understanding, we aim to establish an effective treatment, a mechanism for predictability, and a gold-standard diagnostic test.
The AFE Registry is the comprehensive collection of cases that gather vital information on the efficacy of treatments, and reproductive and long-term health of survivors of AFE, and also serves as a basis for clinical research.
The AFE Biorepository allows for the collection, storage, and examination of blood and tissues from AFE patients. Considerable focus is on the identification of mechanisms of disease and the biomarkers responsible for this syndrome.
The AFE Registry and Biorepository reside at the University of Texas Health Science Center / McGovern Medical School in Houston, Texas.
Specimens We Are Collecting
- Maternal blood that has been previously collected for clinical care before the diagnosis of AFE syndrome (i.e., type and screen)
- Maternal blood was taken during the event but before transfusion
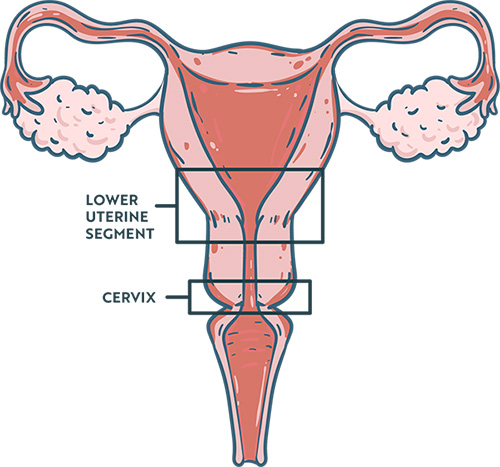
- Pathological specimens from the placenta or surgical pathology specimens (i.e., placenta, uterus, etc.)
- Autopsy specimens (FFPE Tissue Blocks):
- Ectocervix/endocervix
- Lower Uterine Segment full-thickness transmural section
- Brain
- Heart
- 1-2 Sections of each lobe of the lung
How to Submit Specimens
Contact the AFE Hotline at 1-307-363-2337 immediately following a possible or suspected AFE event, and for up to 7 days afterward. For cases beyond 7 days, complete the Submit a Case Form.
Further Reading
"On analyzing 42 autopsy specimens of cases of maternal death, 36% of causes of death by autopsy were discordant with the clinical diagnosis. Moreover, of the 38% of non-autopsied maternal deaths, the cause of death could not be clarified from the clinical chart. Detailed autopsies are necessary to clarify the precise pathologic evidence related to pregnancy and delivery, especially causes of unexpected death such as amniotic fluid embolism.”
Wakasa, T., Ishibashi-Ueda, H., & Takeuchi, M. (2021). Maternal death analysis based on data from the nationwide registration system in Japan (2010-2018). Pathology International, 71(4), 223–231. https://doi.org/10.1111/pin.13076
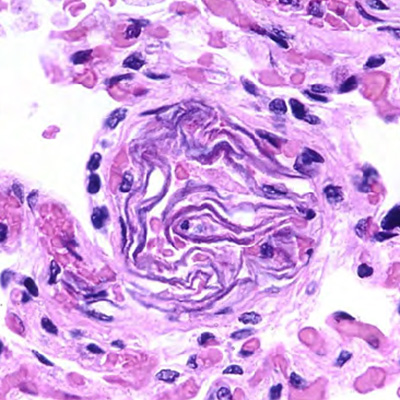
“Amniotic fluid may induce distinct thrombus formation in the uterus and lungs. Pulmonary and uterine thrombi formation may contribute to cardiorespiratory collapse and/or consumptive coagulopathy in AFE.”
Yamashita, A., Oda, T., Aman, M., Wakasa, T., Gi, T., Ide, R., Todo, Y., Tamura, N., Sato, Y., Itoh, H., & Asada, Y. (2023). Massive platelet-rich thrombus formation in small pulmonary vessels in amniotic fluid embolism: An autopsy study. BJOG: An International Journal of Obstetrics and Gynaecology, 130(13), 1685–1696. https://doi.org/10.1111/1471-0528.17532
“All this, moreover, underlines the indispensability of the post-fatal histological examination to reach the correct diagnosis of this entity, which could otherwise go unnoticed. In conclusion, amniotic embolism is unfortunately confirmed as a sudden, severe, and highly lethal obstetric complication even today, which is why both clinicians and forensic pathologists must be aware of it to implement the most appropriate diagnosis from their respective points of view.”
Gentilomo, A., Tambuzzi, S., Gentile, G., Boracchi, M., Andreola, S., & Zoia, R. (2024). Post-mortem diagnosis of amniotic fluid embolism. Autopsy & Case Reports, 14, e2024472. https://doi.org/10.4322/acr.2024.472
“There is a substantial discrepancy between clinical and autopsy causes of maternal death which necessitates asking for an autopsy in cases of maternal mortality of uncertain cause.”
Ghalib Yassin, B. A., Hassan Al-Safi, A. M., & Al-Saneed, E. H. (2022). Autopsy versus Clinical Decisions Regarding Causes of Maternal Death in Iraq. Indian Journal of Community Medicine: Official Publication of Indian Association of Preventive & Social Medicine, 47(2), 177–181. https://doi.org/10.4103/ijcm.ijcm_571_21
“Maternal deaths can pose a particular challenge to the forensic pathologist and carry significant short- and long-term implications for family members and wider medical and legal practice. The role of the forensic pathologist has an important contribution to wider surveillance and research processes that can contribute to changes in clinical practice, policy, and subsequent changes in maternal mortality rates.”
Garland, J., & Little, D. (2018). Maternal Death and Its Investigation. Academic Forensic Pathology, 8(4), 894–911. https://doi.org/10.1177/1925362118821485
“A total of 129 charts were available for review. Of these, 46% (59/129) represented typical amniotic fluid embolism and 12% (15/ 129) atypical amniotic fluid embolism, 21% (27/129) were non-amniotic fluid embolism cases with a clear alternative diagnosis, and 22% (28/129) had an uncertain diagnosis. Of the 27 women misclassified as an amniotic fluid embolism with an alternative diagnosis, the most common actual diagnosis was hypovolemic shock secondary to postpartum hemorrhage.”
Stafford, I. A., Moaddab, A., Dildy, G. A., Klassen, M., Berra, A., Watters, C., Belfort, M. A., Romero, R., & Clark, S. L. (2020). Amniotic fluid embolism syndrome: analysis of the Unites States International Registry. American Journal of Obstetrics & Gynecology MFM, 2(2), 100083. https://doi.org/10.1016/j.ajogmf.2019.100083
More about The AFE Foundation
The Amniotic Fluid Embolism Foundation, a non-profit organization founded in 2008, quickly united the voices of families, survivors, medical professionals, and researchers to call for greater awareness and resources to reduce the threat of amniotic fluid embolism (AFE). Our collective efforts have resulted in an internationally recognized research program on AFE, highly sought-after educational programming for healthcare providers, and a worldwide network of support groups and resources for those impacted by an AFE.
✔️Visit www.afesupport.org for resources for grieving families.